How Long Will Symptoms Of Headache Last Following COVID-19 Infection? How To Remove Long COVID Headache?
- Long Covid Classified Treatment Options
- 05 Nov, 2022
Summary
Headache is common as one of long-term COVID-19 syndrome after COVID-19 infection. Long-term COVID-19 symptoms of headaches sometimes appear during the initial infection, sometimes delays for some time, presenting as intermittent or daily chronic headaches. Daily chronic headaches often appear along with other long-term COVID symptoms, most commonly with hyposmia. A chronic headache is usually characterized by daily chronic migraine headaches, or more commonly tightness of the head, which is also called chronic tension headaches.
By studying the medical papers on chronic headaches in long-term COVID-19 symptoms so far, the authors summarize the life performance of long-term COVID-19 symptoms of headaches and gave an in-house self-assessment to judge whether people developed these symptoms. Then, the analysis of pathogenesis of chronic headache caused by coronaviruses showed that the continuous activation of immune system and the activation of trigeminal nerve vessels were considered to be one of the causes of post-COVID-19 headaches. The authors summarized the therapeutic ideas of western medicine for the disease, finding out that the current treatment is guided primarily by existing guidelines for primary headache with a corresponding phenotype.
Due to the limitation of western medicine treatment against long-term COVID-19 symptoms of headache, this paper also recommended some traditional Chinese medicine, including Chinese medicine formula and acupuncture treatment, to treat the related symptoms of headache. In addition, this paper made advises patients with long-term COVID-19 symptoms of chronic headache on taking health care products, as well as on exercise, diet, and sleep. In the end, we hope that the treatment program for long-term COVID-19 symptoms of chronic headache suggested in this paper could benefit patients by improving their symptoms as soon as possible, and even cure these symptoms of chronic headaches caused by novel coronavirus.
Keywords: Long COVID, Post-COVID Conditions, Post COVID-19 Symptoms, Long COVID headache daily chronic headache, long-term COVID-19 symptoms of chronic migraine, Long COVID headache, long-term COVID-19 symptoms of daily head tightness
1.What Are The Clinical Manifestations Of Long COVID Chronic Headache?
A large proportion of long-term COVID-19 symptoms are associated with brain, and some medical communities use a folk colloquial vocabulary” brain fog” to facilitate the unified classification and description of post COVID-19 symptoms associated with the brain. Brain fog has not previously been regarded as a medical or scientific term, but rather a colloquial description of a state in which people cannot think normally and clearly when they develop influenza or other diseases.
Ordinary people use the fog in their brains to describe problems arising in their usual cognition or thinking, such as difficulty in concentrating, chronic headaches, slower thinking speed, inability to think keenly, lack of creativity, and difficulty in formulating plans. During rehabilitation after being infected with COVID-19, many patients said they experienced "brain fog". According to figures given in the study report, about 1% of patients infected with COVID-19 will experience brain fog.
At present, it has become customary in the medical community to classify chronic headache caused by COVID-19 infection as Long COVID brain fog. According to statistics in the study report, chronic headache patients accounted for a quarter of the overall long COVID brain fog patients. That means about 0.25% of people infected with COVID-19 will experience chronic headaches. According to published medical papers on long-term COVID chronic headache, we conclude that the manifestations of chronic headache are as follows:
(1) Chronic Migraine: feel chronic headache throughout the brain, or symmetrical chronic headache bilaterally in the brain. Sometimes there is rhythmic throbbing pain in sensation.
(2)Chronic tension headache: frequently feel hot head and tightness of head. Some people present with tension headache. Someone may feel like the squeezed brain or tightened brain muscles.
(3)Accompanying symptoms, brain fatigue: feel drowsy, it’s easy for brain to feel tired, feel fatigued when thinking, it’s easy to feel sleepy when reading, feel sleepy in the daytime.
(4)Accompanying symptoms, dizziness: feel a false sense of movement or rotation, vertigo, feel lightheaded, unstable to stand or walk, and likely to loss balance and fall.
(5)Accompanying symptoms, loss of smell: olfactory dysfunction, feel that one can not smell anything through the nose, or that the smell is abnormal.
2.How Long Will Symptoms Of Chronic Headache Last Following COVID-19 Infection?
2.1 What Are Post-COVID Conditions?
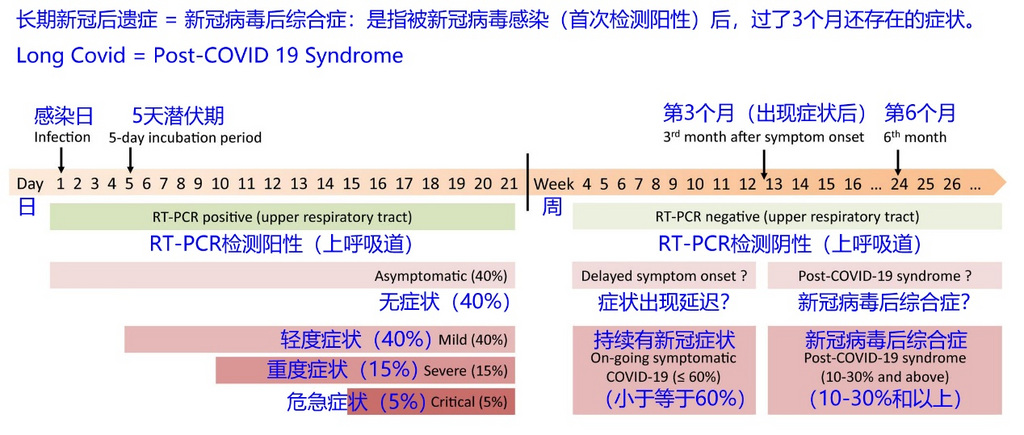
According to the definition of the World Health Organization, Post-COVID Conditions or Long COVID, also known as Post COVID-19 syndrome, refers to since the patient was infected with the novel coronavirus, the results of his PCR showed positive as criteria, and he still suffers uncomfortable symptoms after 3 months. More detailed updated statistical information on the incidence of Post COVID-19 Symptoms according to the timeline can be found in the figure below.
Post-COVID Conditions are mainly concentrated in five aspects, including respiratory syndrome, cognitive system syndrome, chronic fatigue syndrome, chronic pain syndrome, and mental syndrome, such as long-term COVID-19 brain fog, which belongs to the cognitive system syndrome. Long-term COVID chronic fatigue is one of chronic fatigue syndrome.
If you have a history of the novel coronavirus, which means your previous result of PCR test showed positive, and before infection with the novel coronavirus, you didn’t suffer from headaches, but now you are presenting these symptoms of chronic headache in the above section, you are likely to afflict by Post COVID-19 Symptoms of daily chronic headaches.
2.2 How Long Will Symptoms Of Chronic Headaches Last Following COVID-19 Infection?
How long will COVID-19 headaches last? Headaches caused by COVID-19 infection usually last 10 to 14 days. But even after recovery from acute symptoms early in COVID-19 infections, people still feel headaches. A study found that more than half of people still experience chronic headaches for up to six months after illness.
In 2021, in a study designed to describe long-term COVID-19 symptoms in more than 3,000 people from 56 countries, researchers found that 88% of respondents represented brain fog symptoms such as cognitive, headaches, or memory problems. During the first few months after the onset of COVID-19 symptoms, these symptoms showed an increasing trend and then started to decrease gradually. At the beginning of the 7th month after the onset of COVID-19 symptoms, 55.5% of respondents reported suffering from cognitive problems such as brain fog.
A 2022 study investigated the rehabilitation of individuals with neurological symptoms such as long-term COVID-19 brain fog. The mean duration of brain fog since participants developed symptoms of COVID-19 infection was 14.8 months. After an initial evaluation, participants were followed up for 6 to 9 months. During follow-up, no significant changes were observed in the reporting of brain fog symptoms compared with the initial assessment, which means there was no significant change among most patients with brain fog. Researchers still pointed out that the quality of life measures of study participants remained lower than that of the general population.
According to published medical statistics papers on long-term COVID brain fog, the symptoms could last for quite a long time. The symptoms of brain fog tend to peak within a few months of infection with COVID-19 and then generally begin to improve over time. However, brain fog may still persist for several months. Recent studies have found that brain fog symptoms may last more than a year after infection with COVID-19. Moreover, studies have shown that more than 20% of patients with long-term COVID brain fog still did not get an improvement for their symptoms after a year.
3.What Are The Causes Of The Long COVID Chronic Headache?
3.1 What Are The Clinical Manifestations Of New Daily Persistent Headaches Following COVID-19 Infections?
Headache is one of the earliest and most common symptoms in the acute phase of COVID-19, that is, the early phase of infection. According to published studies, approximately 14% to 60% of patients develop headaches early in the course of COVID-19 infection, which manifests clinically as compressive pain in the upper or anterior part of the head.
For patients infected with novel coronavirus, they may have experienced immune cytokine storm and severe fever during the infectious period, because some studies have confirmed that fever is one of a cause of long COVID chronic headaches. Studies have also shown that arterial hypertension occurs after the patients experienced cytokine storm, which is also one of the causes of the long-term COVID chronic headache.
About 18% of people develop new daily persistent headaches(NDPH) three months after becoming infected with COVID-19. A cross-sectional study found that 50% of patients who presented with hyposmia after several months of recovery from SARS-CoV-2 infection had persistent headaches. COVID-19 has been shown to infect the nasal cavity, causing damage to olfactory sensory neurons and resulting in decreased lymphatic circulation in the brain. This suggests that post-COVID-19 chronic headaches may be associated with the olfactory nervous system.
Studies have shown that sometimes the coronavirus infects the eye, causing damage to retinal nerve cells and neurons in the brain, which can also cause chronic headaches. It has also been shown that trigeminal vascular activation is associated with chronic headache following the COVID-19 infection.
Post-COVID-19 symptoms of headaches are characterized by intermittent or chronic new daily persistent headache (NDPH), and there is a significant correlation between the time point of onset of headache symptoms and different time periods of the day in patients, with more cases of headache in the afternoon, and the performance is more difficult to eliminate under treatment. This suggests that post COVID-19 chronic headache is likely to be associated with the body's circadian clock as well as metabolism.
According to two studies, men around the age of 30 have the least chronic headache symptoms, and women around the age of 50 have the most chronic headache symptoms following COVID-19 infection. A multivariate analysis of 576 inpatients followed for one year found that immunocompromised patients had a longer duration of headaches over time (HR 2.9; 95% CI 1.02 – 8.22). This suggests that post-COVID chronic headaches are likely to be associated with the immune system and chronic inflammation in humans.
Most of the headache caused by COVID-19 is similar to that caused by other systemic viral infections and, like other secondary headaches, presenting with bilateral and compressive features, tension-type headache phenotypes are more. It has been shown that people with a previous history of migraine have a 40% increased probability of developing long-term headaches during the late coronavirus infection period. This suggests that post-COVID-19 symptoms of chronic headache are likely to have similar pathogenesis to new daily persistent headache (NDPH) caused by other causes.
3.2 What Is The Pathogenesis Of New Daily Persistent Headache Following COVID-19 Infection?
According to several published research papers, the pathogenesis of long COVID new daily persistent headache (NDPH), is mainly caused by the continuous activation of the immune system of the human body, and neuroinflammation caused by the invasion of the brain by the coronavirus breaking through the blood-brain barrier.
It has been shown that higher cortical surface area and gray matter volume in the orbitofrontal cortex were observed in samples from long-term COVID-19 headache patients, with most changes occurring in areas associated with primary olfactory cortex function. After comparing resting state connectivity between COVID-19 survivors and healthy controls, the researchers observed diminished functional connectivity between the cingulate gyrus, hippocampus, parietal lobe, temporal lobe, and frontal lobe.
In addition to gray matter and connectivity changes, the white matter has also been reported to change in COVID-19 survivors compared to healthy controls. The researchers found higher axial diffusivity in nervous system metabolism in the radiating corona, inner and outer sacs, suggesting some degree of white matter axonal changes. These changes may all be associated with the persistence of headache. Regarding cerebral metabolism, the regions most frequently reported as hypometabolic included the right parahippocampal gyrus, brainstem, thalamus, amygdala, orbital gyrus, olfactory gyrus, and temporal lobe.
In order to enter host cells, novel coronavirus uses the angiotensin-converting enzyme 2 (ACE2) receptor, which has been shown to be expressed in the central nervous system (CNS) and among other regions. More precisely, the expression could be observed in cerebral vessels, monolayer choroid plexus(CP) epithelial cells, and neocortical neurons. This expression pattern suggests that the virus may be able to enter the central nervous system.
Studies have shown that patients infected with COVID-19 can trigger inflammation of the olfactory bulb or even atrophy of the olfactory bulb if the virus further invades epithelial cells in the olfactory bulb, such as capillary epithelial cells, which disrupts the transmission of electrical signals between olfactory neuron cells and mitral neuron cells. Based on the above studies, we can deduce the process of how novel coronavirus invades the brain through the olfactory nervous system.
3.3 The Process Of Novel Coronavirus Invading The Brain Through The Olfactory Nervous System And Leading To Brain Inflammation
The following figure shows how the novel coronavirus invades the brain through the olfactory nervous system and leads to brain inflammation:
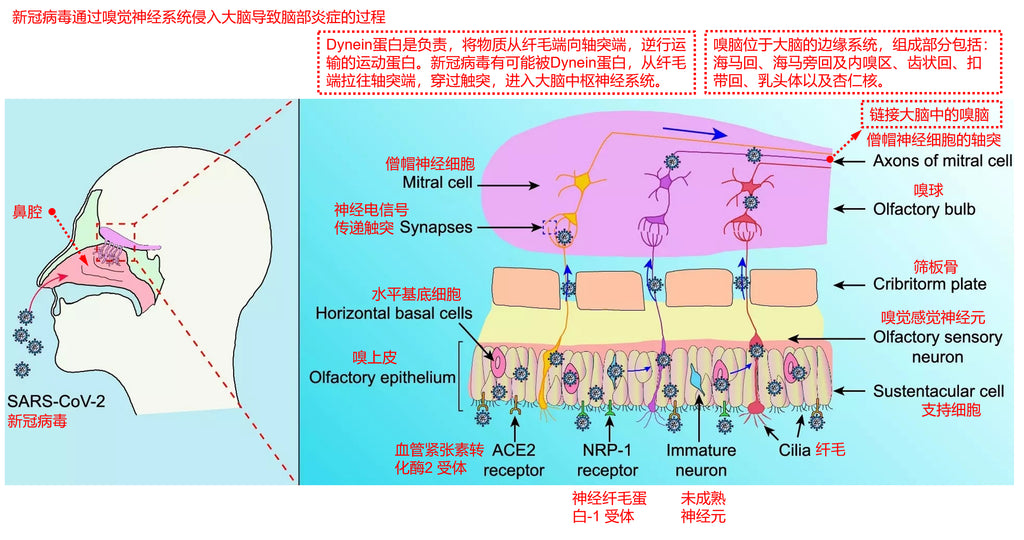
(1) Novel coronavirus enters through the respiratory tract and attaches to epithelial cells of the upper respiratory tract and lungs. The novel coronavirus recognizes host receptors via the spike glycoprotein (S protein) of coronavirus.
(2) It then binds to ACE2 (angiotensin-converting enzyme 2) receptor and TMPRSS2 (transmembrane serine protease 2) receptor and enters Sertoli cells of the olfactory epithelium and horizontal base cells of the olfactory epithelium in a membrane-fused manner.
(3) Extracellular vesicles (EV) are nanoscale membrane vesicles composed of lipid bilayers and secreted by all cell types. They act as carriers, protecting macromolecules such as proteins and RNAs from enzymatic degradation, and transporting these macromolecules between different cells, from adjacent cells to more distant cells, or immune cells. In addition, specific extracellular vesicles (EVs) have been shown to be able to cross the brain barrier.
(4) Very small amounts of novel coronavirus in Sertoli cells of the olfactory epithelium and horizontal base cells of the olfactory epithelium may be encapsulated into extracellular vesicles (EVs) and then enter olfactory neuronal cells.
(5) In neuronal cells, Dynein protein is the motor protein responsible for retrograde transport of substances from the cilia end to the axons end. The novel coronavirus is likely to be pulled from the cilia end of olfactory neurons to the axonal end by the Dynein protein, thereby entering the olfactory bulb.
(6) In the olfactory bulb, olfactory neurons and mitral neurons communicate neuroelectrical signals through touch process connections, at which time novel coronavirus may be encapsulated into extracellular vesicles (EVs) and then into mitral neuron cells.
(7) In mitral neurons, novel coronavirus may be retrogradely transported by Dynein protein into deeper brain neurons and thus enter the central nervous system of the brain.
The brain region connecting the olfactory bulb is called the limbic system of the brain, also known as the olfactory brain. If the virus further invades the olfactory brain, which is the part of the limbic system of the brain that is responsible for the processing of logic operations for the encoding and decoding of olfactory electrical signals, this makes the electrical signals of the olfactory nervous system unable to be normally understood and operated by the brain, which is the cause of cognitive dysfunction and also one of the causes of brain fog symptoms.
3.4 The Process Of Novel Coronavirus Invading The Brain Through The Blood-Brain Barrier Or The Parenchyma Of Ventricular Organs And Resulting In Brain Inflammation
According to the current medical research results and the generally agreed consensus, there may be the following four ways for the novel coronavirus to directly invade the brain:
(1) The coronavirus invades the brain directly through olfactory organ tissues and the olfactory nervous system.
(2) The coronavirus crosses the blood vessels, breaks through the blood-brain barrier, and directly invades the brain.
(3) The coronavirus passes through blood vessels and leaks to the brain at certain weak spots in ventricular organs, where these endothelial cells are not tightly connected and also lack an astrocyte interception barrier.
(4) The coronavirus infects peripheral nerve cells in human organ tissues, and is transported retrogradely to the brain end through the Dynein protein, and then leaks to the brain by latency into extracellular vesicles (EV). This possibility has not yet been fully substantiated.
Section 3.3 of this article explains how coronavirus invades the brain through olfactory organ tissues and the olfactory nervous system. The following article then explains the process of the coronavirus invading the brain through the blood-brain barrier or the parenchyma of ventricular organs, as shown in the following figure:
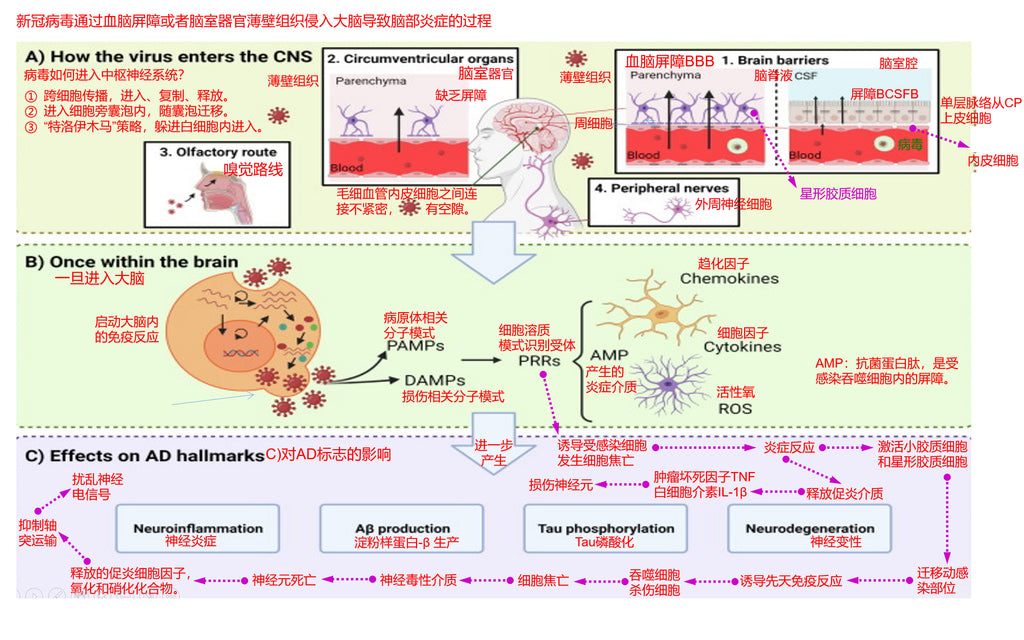
(1) The blood-brain barrier is usually composed of two modes: one is composed of an intercepting network combined of dense astrocytes, and the other is composed of a dense monolayer choroid plexus (CP) epithelial cells to form the blood-brain barrier BCSFB..
(2) The coronavirus is transported to the central nervous system through capillary blood, then infects endothelial cells of microvessels and crosses them, and then breaks through the intercepted network composed of dense astrocytes to enter the brain ventricular lumen.
(3) The coronavirus is transported to the central nervous system via capillary blood and then infects the endothelial cells of the microvessels and crosses them, then infects the monolayer choroid plexus (CP) epithelial cells and crosses them to enter the brain ventricular lumen.
(4) In addition to the blood-brain barrier, novel coronavirus enters the brain ventricular lumen from these loopholes in certain weak spots of ventricular organs, where these endothelial cells are not tightly connected and there is also a lack of astrocyte interception barrier.
(5) Once the coronavirus enters the brain, it begins to invade tissues and organs and central neuronal cells in the ventricular cavity, and start to replicat, proliferation, propagation.
(6) Viral infection activates the immune system in the brain and turns on PAMPs (pathogen-associated molecular patterns) and DAMPs (damage-associated molecular patterns), which in turn produce PRRs (cytosolic pattern recognition receptors).
(7) PRRs (cytosolic pattern recognition receptors) include: Cytokines (cytokines), Chemokines (chemokines), ROS (reactive oxygen species), AMP (antimicrobial protein peptides, which are inflammatory mediators and barrier fragments in infected phagocytes).
(8) At this point, the inflammation of the brain begins to spread.
From the above pathological deduction steps, novel coronavirus infection triggered an inflammatory response in the brain, which in turn produced a series of neurodegenerative lesions, causing long-term COVID-19 symptoms and being the cause of chronic headaches symptoms. When we develop long-term COVID chronic headaches, we must treat it seriously, for chronic headaches will further develop into early Alzheimer's disease or Parkinson's disease. Therefore, medical attention should be sought as soon as possible when symptoms of chronic headaches occur.
4. How To Treat Long-Term COVID Chronic Headache Symptoms?
Chronic headache of Long COVID is more prevalent in middle-aged women, accompanied by long-term COVID symptoms such as fatigue, cognitive dysfunction, and dizziness, as well as hyposmia and insomnia or other sleep disturbances. Cross-sectional studies have shown that the topography of headache is predominantly bilateral, predominantly frontal or periocular, and compressive.
The chronic headache phenotype is highly variable, occurring mostly in the temporal and occipital lobes, and often changes according to the pulse rhythm occur in approximately one-third of patients. Headache of Long COVID often mimic the primary headache phenotype. The two most common phenotypes described are tension-type headache and migraine-like headache.
Migraine-like headache may be associated with nausea, vomiting, photophobia, and phonophobia and exacerbated by daily physical activity, whereas tension-type headache is not exacerbated by daily physical activity and rarely associated with other symptoms.
Patients with a history of headache commonly report worsening headache. Tension-type and migraine-like headache features can also be seen in patients who have no personal history of headache or who have not experienced headache in the acute infection phase.
We should follow this figure to reason when diagnosing chronic headache of Long COVID:
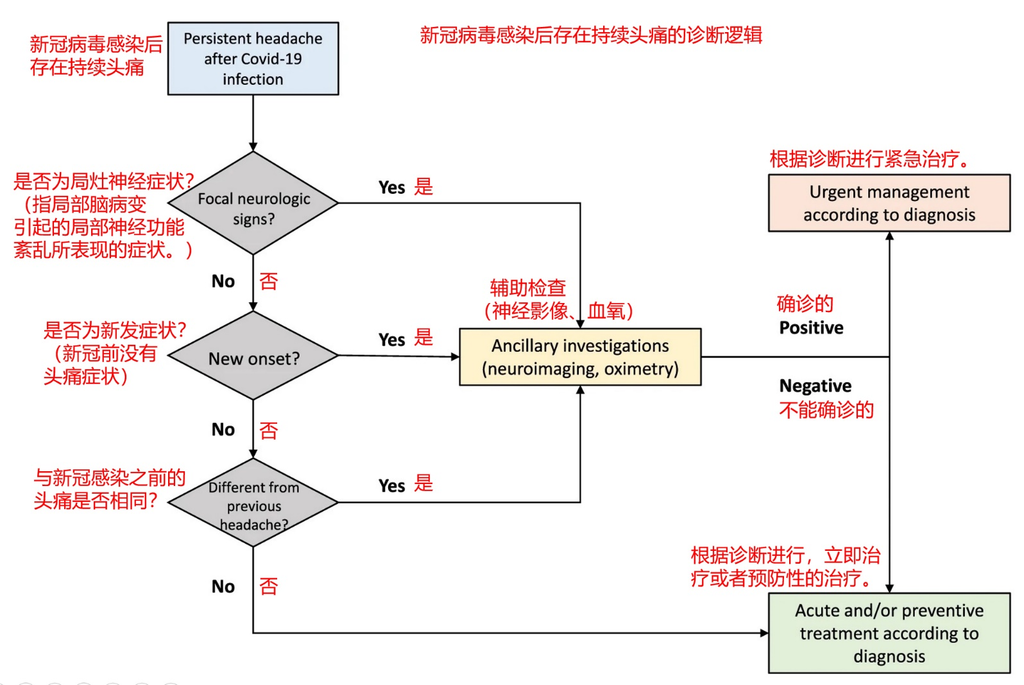
At first, we need to take a thorough physical examination of our bodies, and besides taking routine examinations, we need to do another four examinations.
The first item: do several more PCR tests, and nasal and throat secretions should be dipped enough to check whether the result shows positive. If it shows positive, it means there is still some active novel coronavirus in the body.
The second item: Perform a neurological examination. Because neurological symptoms are highly prevalent in patients with long-term COVID-19, neurological testing is recommended in all patients with long-term COVID-19. Even if some patients communicate with their physicians, they do not have neurologically uncomfortable feedback.
Following unconventional deeper neurological tests can be performed. For example, to rule out testicular brain injury, physicians are advised to perform functional magnetic resonance imaging MRI of the brain, including functional magnetic resonance imaging MR angiography of the brain. In elderly patients, imaging findings of early abnormal brain changes in Parkinson 's disease, Alzheimer' s disease, or other types of neurodegenerative dementia can be excluded by functional magnetic resonance imaging MRI of the brain.
When patients report memory impairment, it is important to determine whether this memory impairment is caused by infection with COVID-19 or whether COVID-19 infection worsens pre-existing symptoms. If ischemic or hemorrhagic stroke is observed on functional magnetic resonance imaging MRI of brain, we must consider medical therapy to prevent recurrent stroke.
Perfusion imaging (single photon emission computed tomography) may also be performed if the patient is wealthy or if the physician suspects the diagnosis. Cerebral perfusion imaging, which is perfusion imaging using CTP and MRP, has become a routine method to examine cerebral blood flow perfusion in stroke patients. Although there is still no evidence that perfusion imaging is an essential test for stroke assessment, many centers have begun to use perfusion imaging to assess cerebral blood flow in patients.
Cerebral perfusion testing may also show the inflammation triggered by non-specific immunity (innate immunity, which refers to the normal physiological defense function congenitally possessed by the body and can make the corresponding immune response to the invasion of various pathogenic microorganisms and foreign bodies) , which is characterized by hypoperfusion in the prefrontal or temporal lobes. Although there is no established treatment for this problem, some drugs that develop brain blood may help improve the condition.
Third item: in addition to basic blood tests, we assessed thyroid hormones, zinc, ferritin, antinuclear antibodies, rheumatoid factor, and blood sedimentation rate in almost all patients. Patients with PASC may have electrolyte disturbances, anemia, thrombocytopenia, hypoalbuminemia, lipid abnormalities, and abnormal glucose metabolism. These data need to be combined with patient symptom descriptions to carefully analyze the pathogenesis behind reasoning to determine whether abnormal laboratory test results can explain the symptoms of PASC.
The fourth item: listen to the sounds of the heart and respiratory system with a stethoscope. Anemia, the signs of heart failure, latent arrhythmias such as atrial fibrillation, and pneumonitis from enteritis must be assessed when abnormal sounds are detected, or if breathlessness persists, and to check whether oxygen saturation decreases during exercise.
The following items, from item 5 to item 7, are required when the patient presents other symptoms.
Fifth item: rheumatoid arthritis or other related diseases must be analyzed when patients have symptoms of joint discomfort.
Sixth item: when the patient complains hair loss, we examine the scalp, return to the history of hair loss symptoms, and confirm the weekly amount of hair loss.
Seventh item: neuropsychological tests should also be performed if the patient has significant psychological problems.
According to the current daily treatment experience of chronic headache, the best treatment is often under the guidance of a doctor, summarized and found out by the patient himself with the most suitable for their own law, covering: work, sleep, diet, exercise lifestyle.
Patients need to record their headache symptoms in detail, that is, to write a diary related to chronic headache symptoms. Headache diaries cover routines before symptom onset, the time point of symptom onset, length of symptom duration, the severity of symptoms, clinical features of symptoms, and routines when symptoms disappear.
Then under the guidance of the doctor, the patient continuously experimentally adjusted his/her: sleep time and sleep length, nap time and nap length, diet before and after sleep and diet ingredients, drinking times per day and water intake per time, working hours, as well as whether rest should be interspersed in the middle of working hours and whether soothing exercise should be interspersed. After a period of adjustment and testing, most people's daily symptoms of chronic headaches will be significantly relieved.
For people with more severe symptoms of chronic headaches, the ideas of designing treatment options are roughly:
(1) According to the results of the patient's comprehensive physical examination and four special examinations as well as the communication with the patient, find out the most likely pathogenesis of the patient's long-term COVID chronic headaches, namely exploring the reason.
(2) Prescriptions are prescribed for treatment according to the pathogenesis and the patient's physical condition.
(3) For the main direction of medication, if COVID-19 remains in the body, antiviral drugs such as Paxlovid are used first. If there is no virus in the body, medication is decided by specific manifestations of symptoms. For example, if people suffer from a mild occasional chronic headache, they can try to take over-the-counter aspirin and Tylenol. Over-the-counter pain medications such as ibuprofen (Advil) and acetaminophen (Tylenol) may also be taken. For chronic tension-type headache, which is the feeling of excessive pressure or tightness in the head, non-steroidal anti-inflammatory drugs (NSAIDs) are the first choice for acute treatment, followed by combination agents including caffeine. Try taking low doses of over-the-counter medications to relieve seizures, soothe blood pressure, and relieve depression. If there is an inflammatory reaction, patients can take some anti-inflammatory drugs such as indomethacin.
(4) For the symptoms that affect the working life of patients, some drugs for the improvement of symptom experience, such as brain strengthening, refreshing, stimulating nerves, and other effects, can also be used according to specific symptoms. Low doses of amitriptyline have been shown to be more effective in patients with post-COVID-19 symptoms of chronic headaches.
(5) Hot or cold compresses can be beneficial if people present with tension headaches. Apply this method on your neck for about 15 to 20 minutes. Oxygen therapy and physical brain massage can also be tried, and studies have shown that these two methods are also beneficial in reducing headache.
(6) If patients suffer from psychiatric symptoms such as insomnia, anxiety, and depression, they should seek help from psychologists and herbalists to eliminate these psychological symptoms. This is also helpful in removing long-term COVID-19 symptoms of chronic headaches.
5.How To Treat Post COVID-19 Symptoms Of Chronic Headaches From a Traditional Chinese Medicine(TCM) Perspective?
From the theory of syndrome differentiation and treatment of TCM, the treatment of long-term COVID-19 symptoms of chronic headaches can obtain more accurate TCM syndrome differentiation and more suitable TCM formulas from the following three steps.
(1) Perform the observation, smelling, hearing, and inquiring of traditional Chinese medicine diagnosis, and consult the comprehensive physical examination report and four special examination reports of western medicine in the previous section at the same time. Only in this way can TCM doctors obtain the most detailed disease information of patients to support them to make the most accurate syndrome differentiation and treatment of patients' conditions.
(2) TCM doctors will classify and summarize the main symptoms, accompanying secondary symptoms, physical condition, and sick parts of the internal organs of the patients according to the most comprehensive disease information of the patients. First, the main symptoms are the most unbearable symptoms of patients at present, such as long-term COVID chronic headaches. Second, accompanying secondary symptoms are that suffered from the main symptoms, which means the patient is experiencing other uncomfortable symptoms, such as brain fatigue, insomnia, anxiety, and depression. Third, to find out the physical condition of the patient, which means the patient's current physical health status, belongs to which category in the TCM constitution. For example, yang-deficiency constitution, phlegm-dampness constitution, qi-deficiency constitution, blood stasis constitution, etc.
(3) TCM doctors, according to the above summary, combined with the internal organs and meridians related to symptoms, comprehensively use the theory and practical experience of TCM to make TCM prescriptions for patients. If acupuncture and moxibustion are required, these programs will also be prescribed.
Traditional Chinese medicine (TCM) theory is mainly based on: Zhang Zhongjing’s “Treatise on Febrile Diseases”, “Synopsis of Golden Chamber”, Huang Yuanyu's “Four Sacred Hearts Source”, “Typhoid Fever Suspension”, “Jinkui Suspension”, “Changsha Yao Jie”, Li Dongyuan 's “Treatise on the Spleen & Stomach”, and Zhang Jingyue' s “Jingyue Quanshu”.
TCM Practical experience, which can be found in Google Scholar (Fig. https://scholar.google.com/), and search for keywords for TCM treatment of long-term novel coronavirus symptoms. For example, COVID-19 Traditional Chinese Medicine, Long COVID Traditional Chinese Medicine. A large number of academic papers on medical research on the treatment of Long COVID by traditional Chinese medicine can be found in this way.
In order to make it easier for everyone to understand the treatment process of TCM, the following is a TCM treatment case of a patient with post COVID-19 symptoms of chronic headaches.
Case 1:
Name: Wang, male, aged 57 years, height 170cm, weight 80 kg.
MEDICAL HISTORY: PCR was positive for novel coronavirus on 10 Mar 2022, followed by typical symptoms of novel coronavirus infection: fever, cough, sore throat, sputum with blood streaks, ageusia, and anosmia. Two weeks later, the symptoms of novel coronavirus infection gradually relieved and disappeared. Later, long-term COVID-19 symptoms of chronic headaches appeared in succession.
Physical examination report of western medicine: (1) PCR test for novel coronavirus showed positive results again.(2) High blood glucose and early symptoms of type 2 diabetes. (3) Brain PET (positron emission tomography, which can determine the occurrence and development of diseases by detecting the metabolic level of the human body) imaging analysis revealed images of decreased metabolic levels. (4) Proinflammatory markers are high and there is slight systemic chronic inflammation. (5) The content of p-tau217 protein in blood is four times higher than that in the average person.
Main symptoms: recurrent chronic headache, feel tight in the head, occasional fever in the head, and occasional dizziness.
Accompanying secondary symptoms: soreness and weakness of the waist and knee, general weakness, anxiety, depression, and depressed mood.
TCM constitution: the body presents phlegm-dampness constitution and blood stasis constitution.
TCM diagnosis evaluation: The body before the novel coronavirus was in a sub-health state, obesity, and following the infection with novel coronavirus, the sub-health state deteriorated, presenting phlegm-dampness congestion, chronic headache, and other symptoms.
The prescription was given by the TCM:
(1) Gastrodia elata headache tablets are used to reduce chronic headache and are used to treat partial headache caused by blood stasis.
(2) Mai luo tong capsules are used to dredge meridian vascular congestion.
(3) Chaihu plus Longgu oyster Tang are used to improve insomnia anxiety.
(4)Qingtan Yizhi Tang is used to remove phlegm and dampness and refresh the brain.
Acupuncture program given by the TCM: electricity is exerted to heat the moxibustion apparatus, and apply moxibustion at the following acupoints.
(1) Baihui, Neiguan, Taixi, and Yongquan points are stimulated by moxibustion to improve cerebral blood circulation and metabolism.
6. Which Kind Of Health Care Products Are Beneficial To Improving Long-Term COVID Chronic Headache?
Taking the patient above as an example, we give the following health product recommendations based on her condition:
(1) Omega 3 (Ω3) fatty acids, containing high amounts of DHA and EPA, are used to improve brain function and protect against cardiovascular and cerebrovascular diseases.
(2) Comprehensive vitamins, mainly VC, VD, and VB, are used to scavenge free radicals, anti-oxidation, and reduce systemic chronic inflammation.
(3) Curcumin is used to scavenge free radicals, anti-oxidation, activate NRF2, and reduce systemic chronic inflammation.
(4) Sulforaphane is used to scavenge free radicals, anti-oxidation, activate NRF2, and reduce systemic chronic inflammation.
(5) Melatonin is used to improve sleep quality.
(6) American ginseng is sliced for making tea or taken American ginseng capsules to replenish qi.
7. What Exercises Are Beneficial To Improving Long-Term COVID-19 Symptoms Of Chronic Headache?
Taking the patient above as an example, we give the following exercise advice based on his condition:
(1) Take moderate aerobic exercise at least three times a week, such as walking, yoga, and stretching, to remove phlegm-dampness.
(2) With the utility of gym equipment, strength training is performed for the major muscle group to improve insulin activity and lower blood glucose.
(3)Use essential oils to refresh the brain and assist with head massage.
8. What Is Beneficial To Improving Long-Term COVID-19 Brain Fog In Terms Of Diet And Sleep?
Taking the patient above as an example, we give the following diet and sleep advice based on his condition:
(1) Control carbohydrate intake, which means reducing the amount of staple food such as rice and noodle, to control animal fat intake.
(2) Do not take any food after lunch, and have breakfast and lunch only a day. Losing weight at least more than 10% of body weight, which means losing 8 kg, reducing the degree of obesity.
(3) Bathing until slightly sweating before sleeping, and lie in bed to do general muscle tightness and relaxation training, improving sleep quality.
9.Patients With Long-Term COVID Chronic Headache Are Welcome To Contact With Our Long COVID Care Center
If there are similar symptoms among readers, contact our Long COVID Care Center for assistance.
Phone: +852 5765 5768
Whatsapp: +852 5765 5768
WeChat: longcovidcarecenter
Email: support@longcovidcarecenter.org
【Disclaimer: The treatment of diseases is a very complex and professional affair. Due to the limitation, Long COVID Care Center can only carry out remote simple interviews, unable to face-to-face offline interviews and obtain comprehensive physical examination results. Therefore, the suggestions, guidance, protocols, and documents conveyed by Long COVID Care Center to patients can only be used as a reference for patients to understand their diseases in many aspects, but cannot be directly used as a treatment plan. Patients must discuss their symptoms with doctors in local hospitals through face-to-face communication. After the patients completed the physical examination required by doctors, they would get a prescription issued by doctors and get the treatment under the guidance of doctors. Therefore, Long COVID Care Center hereby declares that our center is completely exempted from liability when any adverse consequences are caused by self-treatment of the patient for applying any contents convoyed by the center, that is, we do not bear any responsibilities.】


